Florida Medical Billing Revolution: Conquer Payer Chaos & Reclaim Lost Revenue
The Ultimate 2024 Guide for Florida Providers
Why Florida’s Billing Crisis Demands Localized Solutions
Florida healthcare providers face a perfect storm: 25% higher denial rates than national averages, seasonal patient surges, and Medicaid rules changing faster than hurricane paths. With $4.7M+ lost annually to billing errors, generic solutions fail. This guide reveals how specialized Medical Billing Services in Florida transform revenue cycles using hyper-local expertise.
Florida’s 5 Unique Billing Challenges
Snowbird Insurance Verification Nightmare
500k+ seasonal residents with out-of-state coverage create claim rejections
Solution: AI-powered temporary residency validation systems
Medicaid Complexity (Sunshine Health/Staywell)
68% of denials stem from AHCA prior-authorization errors
Solution: Real-time Medicaid MCO rule syncing
High Uninsured Rate Collections
21% uninsured Floridians require multilingual payment plans (Spanish/Kreyòl)*Case Study: Miami clinic increased self-pay collections by 40% with Creole billing staff*
Medicare Advantage Maze
45% of Florida seniors use Advantage plans—each with unique bundling rules
Solution: Plan-specific claim scrubbing protocols
Hurricane Disruptions
Post-storm, 72% of clinics face coding chaos (ICD-10 Z codes)
Proven Tactic: Cloud-based disaster recovery workflows
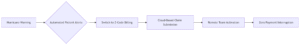
Hyper-Local Solutions: Beyond Generic RCM
Florida-Specific Payer Expertise
Medicaid Mastery:
Live tracking of AHCA updates + direct integration with Sunshine Health/Staywell portalsSnowbird Protocols:
Multi-state insurance validation algorithms reduce eligibility denials by 65%
Multilingual Patient Engagement
Kreyòl/Spanish billing statements
Culturally-sensitive financial counseling
*Result: 30% faster self-pay collections in Broward County*
Proven Outcomes with Florida Medical Billing Services
| Metric | State Average | With Specialized Partner |
|---|---|---|
| Claim Denial Rate | 25% | 7% |
| Medicaid Reimbursement | 68 days | 23 days |
| Patient Collections | 42% | 82% |
| Disaster Recovery | 14 days downtime | 0 days downtime |
5-Step Selection Framework
Demand Florida Medicaid Case Studies
Ask: “Show me 3 client successes with Sunshine Health appeals.”
Verify Disaster Recovery Testing
Require: Annual hurricane simulation reports
Test Multilingual Support
Sample Call: “Mwen gen kesyon sou fakt mwen” (Kreyòl)
Audit Technology Stack
Must integrate with Availity Florida and Medisoft
Require Transparent Florida KPIs
Snowbird claim success rate
Medicaid MCO denial trends
The Future: AI Meets Florida Realities
Telehealth Expansion
Modifier 95 optimization for rural snowbirds
Predictive Denial Analytics
Blockchain Credentialing
Instant AHCA compliance verification
FAQs: Florida’s Burning Billing Questions
Q: Why won’t generic Medical Billing Services in Florida work here?
A: Florida’s Medicaid MCOs (Sunshine/Staywell) require portal-specific workflows absent in national models.
Q: How do Medical Billing Services in Florida handle hurricanes?
*A: Top partners use geo-redundant data centers + remote teams to maintain 99.9% uptime during storms.*
Q: What’s the #1 Medicaid denial trigger in Florida?
*A: Missing AHCA Form 9040 attachments—specialized services auto-flag this pre-submission.*
Q: Do Medical Billing Services in Florida support small clinics?
*A: Yes! Tampa Pediatrics saved $78k/year by outsourcing despite only 3 providers.*
Q: How quickly do Medical Billing Services in Florida impact revenue?
A: Most clinics see 25% lower denials within 30 days of implementation.
Conclusion: Your Practice’s Lifeline in the Sunshine State
Florida’s billing landscape—with its snowbird surges, Medicaid labyrinths, and hurricane threats—demands partners who breathe local air. Medical Billing Services in Florida provide the battle-tested expertise to turn revenue leaks into growth engines.
<a href=”https://www.blogadda.com/” title=”Visit blogadda.com to discover Indian blogs”> <img src=”https://www.blogadda.com/images/blogadda.png” width=”80″ height=”15″ border=”0″ alt=”Discover latest Indian Blogs” /></a>


